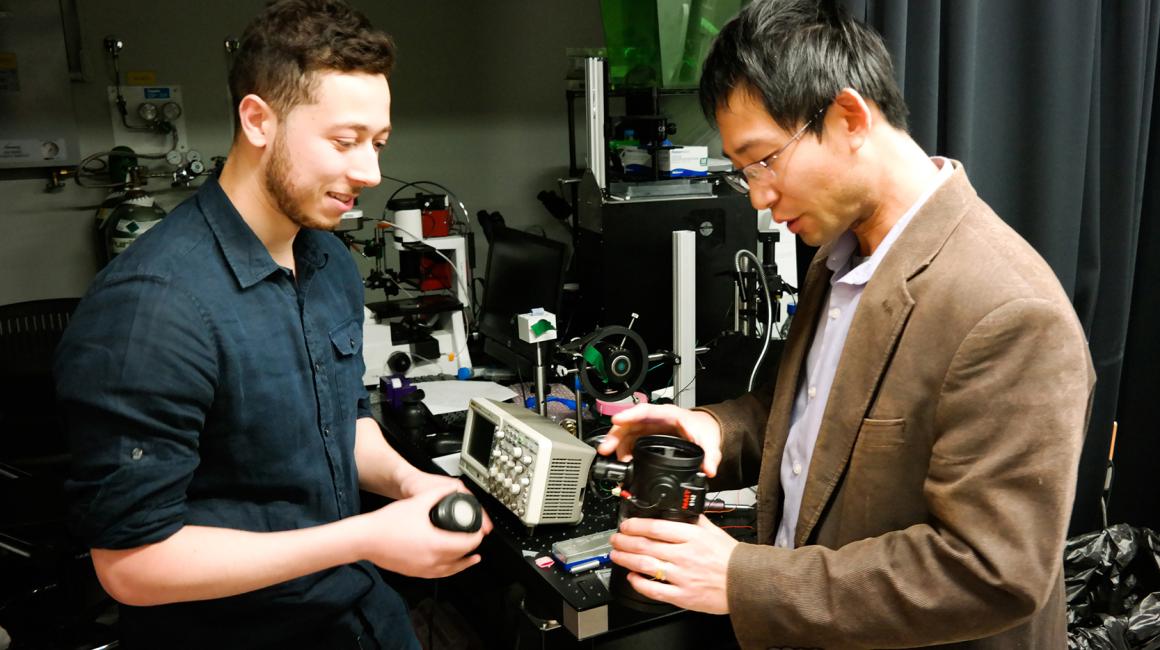
Samer Habeel knows he lucked out scoring a research spot in Mechanical Engineering Assistant Professor Joe Lo’s bioengineering lab. It’s not every undergrad, after all, who gets to hack a high-powered, military-grade riflescope and help turn it into a medical device.
“It’s true: I don’t think many pre-med students are paid to take apart a night vision goggle and hook up high voltage to it,” Lo said, laughing. “But if you use the same standard equipment that everyone else is using, then you’re not going to be able to innovate.”
Lo and Habeel hope their out-of-the-box approach will help them build a prototype device that harnesses the power of ultraviolet light to differentiate between different types of tissues. “It’s really not that far-fetched an idea,” Lo said. “If you’ve been to a night club, you’ve probably seen how black lights make your t-shirt glow blue. That’s because the cotton fibers are being exposed to UV light.”
Other biological materials also fluoresce, though they each have unique color profiles. Habeel and Lo are looking at collagen fibers—a protein that is found in our cells in a variety of forms.
“For example, an ulcer that is not healing or a certain type of skin cancer will have different collagen than healthy tissue. So the idea is different kinds of tissues could be identified based on how they respond to UV light.”
They’re using this concept—and the powerful detectors in that night vision scope—to build two versions of their instrument.
One functions more like a traditional microscope and looks at biopsied tissue samples that are placed on slides. The second version wouldn’t require any tissue samples at all: A medical practitioner could, for example, simply hold the device over a person’s skin, take a scan and get a detailed readout of what a particular tissue was made of.
“The major advantage is that it’s totally non-invasive,” Habeel said. Plus, both devices potentially could provide in-office results within 30 minutes or so. Right now, tissue samples usually require overnight analysis.
Habeel, who expects to graduate this fall, said the project has been a natural blend of his two academic interests. “I’m currently doing a bioengineering degree, but I’m interested in going to medical school,” he said. “This bridges the gap: We’re doing real engineering work with the scope, but the idea is that we want to turn that into something that can be used with actual patients.”
Lo said that kind of innovative mindset is what medical schools are increasingly looking for in students.
“If Samer decides that’s what he wants to do, the technology five years down the line will be a lot different,” Lo said. “So it makes no sense to simply train them with textbooks that are 10 years old, versus an open mind and the experience of discovering new technology. Then he has the motivation and aptitude to figure out what’s next.”
Plus, Lo said, any day he can do something meaningful with a student—with or without a major breakthrough—is a good day in the lab.





